Abstract
Introduction:
There is no direct correlation between the dysplastic features in the bone marrow as well as bone marrow cellularity with the degree of cytopenias in the peripheral blood in patients with MDS. Furthermore, the impact of the percentage of erythroid precursors in the bone marrow has been the subject of considerable debate over the past several decades. We therefore were interested in the prognostic impact of the percentage of erythroid cells in the bone marrow (bmery) for MDS patients. We analyzed the prognostic impact of the amount of erythroid cells in the bone marrow with regard to overall survival and AML evolution, both as single feature and in addition to the IPSS-R.
Methods:
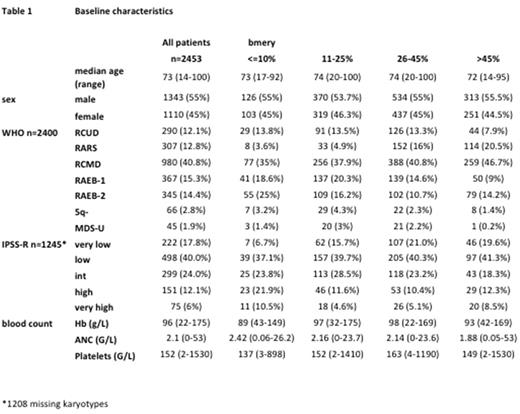
Data from 2453 primary untreated MDS patients from Germany, France, Italy, and Austria with available percentage of erythroid cells in the bone marrow at the time of diagnosis were analyzed. Excluding CMML, the WHO2008 subgroups were RCUD 12%, RARS 13%, RCMD 41%, RAEB-1 15%, RAEB-2 14%, others 5%.
Results:
The median age of the entire patient cohort was 73 years (range: 14-100 years). After a median follow up of 72 months, 1502 patients have died. At the time of data analysis, 282 patients showed a progression to AML. Baseline characteristics are shown in table 1. To evaluate the influence of the percentage of erythroid bone marrow cells on prognosis, we grouped the percentage of cells in <=10%, 11-25%, 26-45% and >45% and found in univariate analysis different median survival rates. OS for bmery <=10% was 23.0 months, for 11-25% 39.9 months, for 26-45% 49.4 months, and for >45% 41.5 months, respectively. Therefore the following three risk categories were defined: "<=10%" (poor), "11-25 or >45%" (intermediate), and "26-45%" (good). Categorized that way, bmery shows prognostic impact on survival (Dxy=0.08, p<0.001) and time to AML progression (Dxy=0.15, p-value <0.001). Taking into account the IPSS-R (by stratified analyses), the Dxy was 0.09 for survival, and 0.18 for transformation, both with p<0.001. Added to the IPSS-R, bmery slightly enhances the prognostic power for both survival (Dxy=0.39) and time to AML (Dxy=0.59). Bmery seems to be more important for time to AML progression, in particular in IPSS-R lower risk categories, but this interaction is not significant. On the other hand, subtracting the bmery from total nucleated cells when calculating the bone marrow blast percentage does not enhance the prognostic power of the IPSS-R. Dxy fall from survival: 0.37 and time to AML: 0.58 to 0.36, and 0.52, respectively. Looking at the peripheral blood count, we could not find a correlation between the percentage of bmery and hemoglobin levels, ANC or platelet count.
Conclusion:
Survival and time to AML progression differ according to the amount of erythroid cells in the bone marrow although we could not demonstrate a correlation between bmery and peripheral blood counts, especially hemoglobin levels. Longest survival and time to AML is found at approximately the normal range of bmery between 26% and 45%. Lower, as well as higher percentages are unfavorable. This u-shaped influence has to be taken into account, when studying prognostic power. Adding bmery as differentiating feature to the IPSS-R may enhance especially the prognostic power for time to AML in lower risk categories.
Fenaux: Janssen: Honoraria, Research Funding; Astex: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Celgene: Honoraria, Research Funding; Janssen: Honoraria, Research Funding; Novartis: Honoraria, Research Funding; Astex: Honoraria, Research Funding. Germing: Janssen: Honoraria; Novartis: Honoraria, Research Funding; Celgene: Honoraria, Research Funding. Nachtkamp: Celgene: Other: Travel Support. Sperr: Amgen: Consultancy, Honoraria, Research Funding; Phadia: Research Funding; Meda: Research Funding; Celgene: Consultancy, Honoraria; Teva: Honoraria; Novartis: Other: Register. Stamatoullas: Takeda: Consultancy; Celgene Corporation: Honoraria. Valent: Celgene: Honoraria, Research Funding; Incyte: Honoraria; Teva: Honoraria; Blueprint: Research Funding; Deciphera: Honoraria, Research Funding; Pfizer: Honoraria; Ariad: Honoraria, Research Funding; BMS: Honoraria; Novartis: Honoraria, Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.